Are you living in constant pain because of uterine fibroids? The heavy bleeding and pressure are exhausting, but the thought of invasive surgery and potential risks creates even more anxiety. You are not alone in fearing the laparoscopic myomectomy risks and complications. Fortunately, there is a way to regain your health without going under the knife.
Understanding the Real Risks of Myomectomy
When you sit down with a doctor to discuss uterine fibroids, the conversation often jumps straight to surgery. Whether it is an abdominal incision or a keyhole procedure, the goal is to remove the fibroids. However, it is crucial to look beyond the “routine” label and understand what this operation actually involves.
Every surgery carries risks. Even with a skilled surgeon, myomectomies are invasive procedures that physically cut into the uterus. While the goal is preserving fertility, the surgical trauma to the uterine wall can lead to unforeseen issues. We need to have an honest discussion about what happens inside the operating room and, more importantly, what happens during the recovery phase.
While many women are told they have a low rate of complications, “low” does not mean zero. For the patient experiencing them, those statistics become a life-changing reality.
laparoscopic myomectomy risks and complications
Laparoscopic surgery, often called minimally invasive or keyhole surgery, is frequently marketed as the “easy” option. While the incisions are smaller than open surgery, the internal work is still major.
One of the most significant risks is intraoperative bleeding. The uterus is a highly vascular organ, meaning it has a rich blood supply. When a myoma (fibroid) is cut out, bleeding can be difficult to control. In some cases, if blood loss becomes excessive, the surgeon may be forced to convert the procedure to an open abdominal surgery or, in very rare and extreme cases, perform a hysterectomy to save the patient’s life.
Furthermore, laparoscopic myomectomy complications can extend to damage of surrounding organs. The bladder, bowel, and ureters are in close proximity to the uterus. During the dissection or use of thermal energy tools to stop bleeding, accidental injury to these organs can occur. These injuries might not be immediately obvious during the operation but can lead to severe infection or peritonitis days later.
Another controversial aspect involves morcellation. This is a technique where the fibroid is cut into smaller pieces to be removed through small incisions. There has been significant medical debate regarding the complication risks of laparoscopic morcellation, specifically the potential to spread undetected abnormal cells throughout the abdominal cavity.
Laparoscopic Myomectomy Recovery
Recovery is often the most underestimated part of the planning process. Patients are frequently told they can return to work quickly, but the body needs time to heal deep internal wounds.
What to expect:
- Pain Management: You will likely need significant pain medication for the first few days to manage pain at the incision sites and from internal healing.
- Physical Limitations: heavy lifting and strenuous activity are restricted for weeks.
- Fatigue: The body uses a lot of energy to repair tissues, leading to tiredness.
- Digestive Issues: Anesthesia and abdominal surgery can slow down the bowel, causing bloating and discomfort.
While the external scars of a laparoscopic procedure are small, the uterus itself has been cut and stitched. Complete healing of the uterine muscle takes months, which is a critical factor if you are planning a future pregnancy.
Types of Myomectomy

Understanding the types of procedures helps in analyzing the risk. The selection of the type usually depends on the size, number, and location of the fibroids.
- Abdominal Myomectomy (Open Surgery):
This involves a large incision (like a C-section). It is usually reserved for very large fibroids. It allows the surgeon to feel the tissue directly but comes with a much longer recovery, higher blood loss, and more pain. Open surgery is widely considered the most invasive option. - Laparoscopic Myomectomy:
As discussed, this uses small incisions and a camera. It requires advanced skills from the surgeon. However, it often leads to longer surgeries compared to open procedures because stitching the uterus laparoscopically is technically difficult and time-consuming. - Hysteroscopic Myomectomy:
This is performed through the vagina and cervix. It is only an option for submucosal fibroids (those inside the uterine cavity). It has fewer risks but is not suitable for the majority of women who have fibroids growing within the muscle wall or on the outside of the uterus. - Robotic Myomectomy:
Similar to laparoscopic, but the surgeon uses a console to control robotic arms. While precise, it still carries the same inherent surgical risks of anesthesia, bleeding, and organ injury.
Adhesions and Long-Term Effects
One of the silent enemies of pelvic surgery is the formation of adhesions. Adhesions are bands of scar tissue that form between organs. After a myomectomy, the raw surface of the healing uterus can stick to the bowel, bladder, or ovaries.
This can cause chronic pelvic pain, intestinal blockage, and ironically, fertility issues—the very thing many women are trying to protect. If the fallopian tubes become blocked by scar tissue, natural conception becomes difficult. Discussion about adhesions is often skipped during the initial consultation, but it affects a significant percentage of patients.
Fertility and Pregnancy Risks
Many women undergo myomectomy specifically to improve fertility. However, the surgery itself poses risks to future pregnancy.
When the uterine wall is cut, it creates a weak point. During labor, the strong contractions required to deliver a baby can put immense pressure on this scar. This leads to an increased risk of uterine rupture, a catastrophic event where the uterus tears open, endangering the life of both the mother and the baby. Because of this potential danger, most women who have had a deep myomectomy will be required to have a C-section for all future deliveries to reduce the risk of rupture during labor.
How Fast Do Fibroids Grow Back After Myomectomy?
This is the question every patient should ask. Surgery removes the visible fibroids, but it does not treat the underlying cause.
Recurrence rates are frustratingly high.
Research suggests that new fibroids can grow back within a few years. Studies indicate that up to 30-50% of women may experience recurrence within 5 years following surgery.
- Why? The hormonal imbalance and genetic factors driving fibroid growth remain active.
- The Result: Many women find themselves facing a second or third surgery down the line. This cycle of surgeries increases the cumulative risk of scar tissue and complications.
Anemia and the Pre-operative State
Many patients suffer from severe anemia due to heavy periods before they even get to the hospital. Operating on an anemic patient increases the surgical risk. Doctors often try to boost iron levels before surgery, but if bleeding is severe during the operation, an anemic patient tolerates it poorly, increasing the likelihood of needing a blood transfusion.
The Conservative Approach vs. Invasive Surgery
Is there a conservative way to treat fibroids that doesn’t involve cutting? Yes.
Modern medicine has shifted towards minimal invasive techniques that focus on treating the organ without physically traumatizing it. We need to move away from the mindset that “cutting it out” is the only cure. The outcomes of non-surgical treatments have proven that you can get relief without the downtime or the scars.
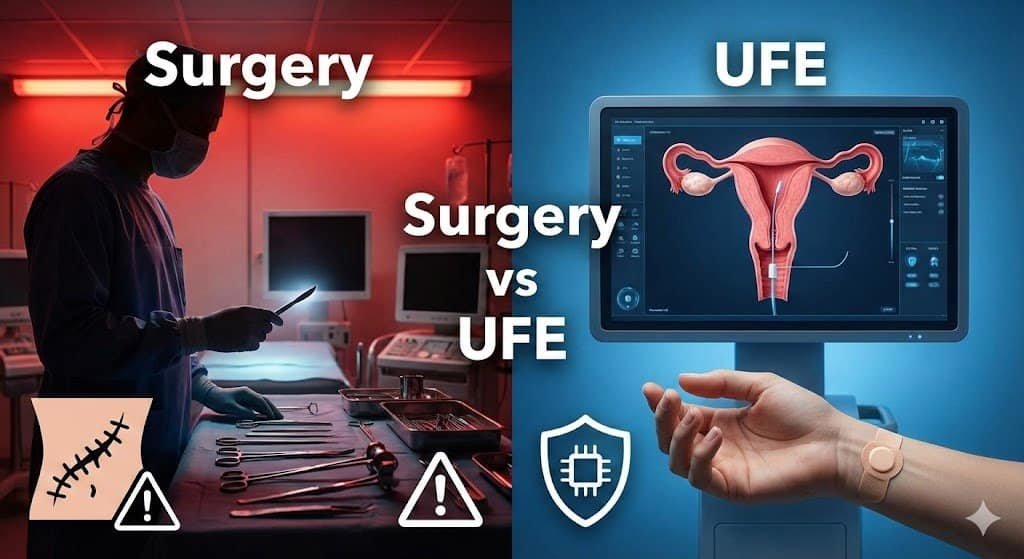
Which is Better, UFE or Myomectomy?
This comparison is vital for your decision-making analysis.
Myomectomy (Surgery):
- Pros: Removes the fibroid immediately.
- Cons: General anesthesia, surgical incisions, risk of infection/bleeding, long recovery (4-6 weeks), risk of adhesions, risk of uterine rupture in pregnancy, high recurrence rate.
- Hospital Stay: Usually 1-3 days.
Uterine Fibroid Embolization (UFE):
- Pros: No general anesthesia, no surgical incisions (only a tiny pinhole), uterus remains intact, treats ALL fibroids at once, very short recovery (approx. 1 week), no risk of surgical adhesions.
- Cons: Post-procedure cramping (managed with medication).
- Hospital Stay: Same-day discharge or one night.
When you weigh the gains, UFE stands out as the superior choice for women who wish to avoid the trauma of surgery while effectively treating their symptoms.
Why UFE is the Best Modern Treatment for Fibroids

Uterine Fibroid Embolization (UFE), performed by an Interventional Radiologist like Dr. Samir Abdel Ghaffar, uses advanced imaging to treat fibroids from the inside out.
How it works:
Instead of cutting the uterus, Dr. Samir inserts a thin catheter into the artery through a tiny nick in the skin (usually the wrist or groin). He guides this catheter to the uterine arteries that supply blood to the fibroids. Tiny particles are injected to block this blood supply.
Why it is a game-changer:
- Starves the Fibroids: Without blood, the fibroids shrink and die.
- Comprehensive Treatment: It treats all fibroids present, even the tiny ones that a surgeon might miss during a myomectomy. This significantly lowers the chance of recurrence.
- Preserves the Uterus: There is no cutting, sewing, or scarring of the uterine wall.
- Quick Recovery: Most women are back to their normal lives within a week 🌿.
This procedure explains why modern healthcare is moving away from dependent surgical methods toward intelligent, image-guided interventions. It offers benefits that surgery simply cannot match.
Dr. Samir Abdel Ghaffar: Expert Care Without Surgery
Dr. Samir Abdel Ghaffar is a renowned Consultant in Interventional Radiology. He specializes in treating uterine fibroids and adenomyosis using uterine artery catheterization (UFE).
His approach is rooted in the belief that women should not have to sacrifice their physical well-being or face the high risks of myomectomy to get relief. By using state-of-the-art technology, he ensures that patients receive the most effective, safe, and updated treatment available globally.
Choosing Dr. Samir means choosing a path that respects your body. It avoids the operative dangers and ensures you are back on your feet, living your life, in a fraction of the time surgery would require.
FAQs
What are the risks of laparoscopic myomectomy?
The risks include excessive blood loss requiring transfusion, accidental injury to the bladder or bowel, infection, formation of internal scar tissue (adhesions), and potential complications related to general anesthesia.
Is laparoscopic surgery considered high risk?
While it is minimally invasive compared to open surgery, it is still major surgery. For women with very large or numerous fibroids, or those with previous surgeries, the risk profile increases. The potential for conversion to open surgery or inadvertent organ damage classifies it as a procedure requiring serious consideration of alternatives.
What is the most common problem following a myomectomy?
The most common problems are recurrence of fibroids (growing back) and the formation of pelvic adhesions. Adhesions can cause long-term pain and fertility issues. Immediate post-op issues often include pain and fatigue.
What are the contraindications for laparoscopic myomectomy?
Contraindications may include having very large fibroids (typically larger than 10-12 cm), multiple fibroids that would require excessive operating time, suspected malignancy (cancer), or patients with medical conditions that make prolonged anesthesia dangerous.
Your health is your most valuable asset. Don’t let the fear of surgery dictate your future. There is a safer, non-surgical path waiting for you.
Contact Dr. Samir Abdel Ghaffar today to discuss if UFE is right for you. 🩺
1. Contact the following numbers in London, UK:
- Clinic number: 00442081442266
- WhatsApp number: 00447377790644
2. Contact the following numbers in Egypt:
- Cairo booking number: 00201000881336
- WhatsApp number: 00201000881336
 العربية
العربية 

